According to new research published in the journal Gut, the composition of the gut microbiome may influence the magnitude of the immune response and disease severity in patients with coronavirus disease-19 (COVID-19) (1).
COVID-19 is primarily a respiratory disease, however, mounting evidence suggests gastrointestinal tract involvement. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can enter and replicate in human enterocytes (2), and the virus is detected in up to 50% of faecal samples (3,4). Several recent studies demonstrate altered gut microbiota composition in infected patients (5,6), and elevated faecal calprotectin, indicating an intestinal inflammatory response (7).
Given the gut microbiome's role in regulating the immune-inflammatory response, the researchers sought to examine the potential link between the gut microbiome and disease pathophysiology.
In this two-hospital cohort study, serum samples for inflammatory markers and stool samples for microbiome composition were collected from 100 hospital in patients with laboratory-confirmed SARS-CoV-2 infection. More than 50% of patients were classified as having moderate to critical disease severity. Eleven patients had hypertension, but fewer than five patients had any other comorbidity.
To characterise the gut microbiome, 41 of the COVID-19 patients provided multiple stool samples during hospitalisation, 27 of whom provided serial stool samples up to 30 days after clearance of SARS-CoV-2.
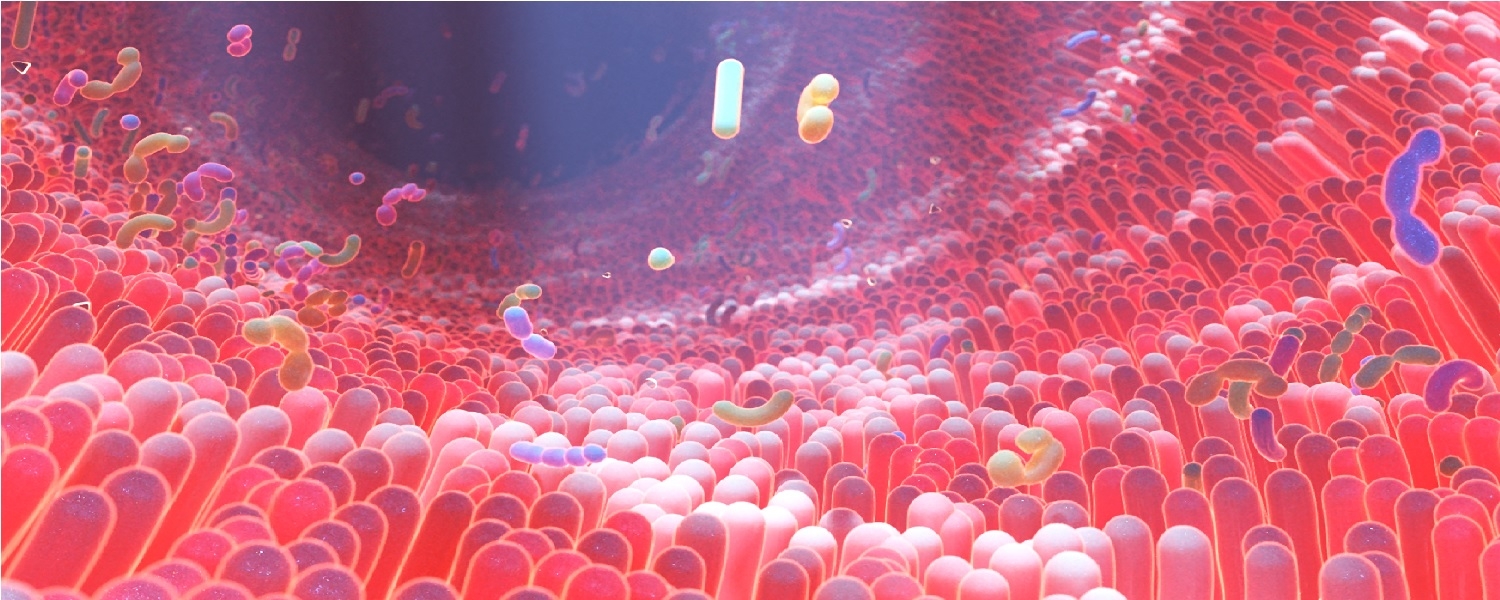
Gut microbiome compositions were characterised by shotgun sequencing ![]() of total DNA extracted from stools and compared to a non-COVID-19 control cohort of 78 adults. In the control cohort, hypertension was the only significant comorbidity, occurring in 11 individuals.
of total DNA extracted from stools and compared to a non-COVID-19 control cohort of 78 adults. In the control cohort, hypertension was the only significant comorbidity, occurring in 11 individuals.
The gut microbiome composition differed significantly between individuals with and without COVID-19, irrespective of whether patients received medication, including antibiotics and antivirals.
Compared to adults without COVID-19, infected patients had higher numbers of inflammatory-associated gut microorganisms, including Ruminococcus gnavus, Ruminococcus torques, and Bacteroides dorei, and lower numbers of species with known immunomodulatory potential, including Faecalibacterium prausnitzii, Eubacterium rectale, and several bifidobacteria species.
F. prausnitzii and Bifidobacterium bifidum were negatively correlated with disease severity after adjusting for antibiotic use and patients' age.
These beneficial gut commensals remained depleted in samples collected up to 30 days after disease resolution, irrespective of whether patients had received antibiotics, suggesting a possible correlation with post-viral infection symptoms and inflammation.
SARS-CoV-2 infection is accompanied by an antiviral immune response involving the release of inflammatory cytokines. An aberrant or exaggerated immune response produces an excessive inflammatory reaction, known as the cytokine storm, in some individuals (8). Patients with severe COVID-19 consistently exhibit high blood plasma levels of inflammatory cytokines and markers such as IL-6, -8, -10, TNF-α, and C reactive protein (CRP), reflecting the exaggerated immune response and tissue damage (9,10).
In the current study, the gut microbiota composition of COVID-19 patients during hospitalisation was correlated with disease severity and plasma concentrations of inflammatory cytokines, chemokines, and blood markers of tissue damage. Specifically, the depletion of several known immunomodulatory bacterial species, including F. prausnitzii and E. rectale, was linked to increased concentrations of inflammatory markers (e.g. IL-10 and TNF-α).
The study does not account for confounders such as the heterogeneity in clinical management, and presence of comorbidities. Furthermore, the study is observational, so cannot establish whether variation in the gut microbiome is determining COVID-19 severity or is a consequence of the infection on the gut and the immune system.
However, given the mounting evidence that gut microorganisms are linked to inflammatory diseases (11), studies are urgently required to understand the specific roles of gut microbiota in the immune-inflammatory response to SARS-CoV-2 infection.