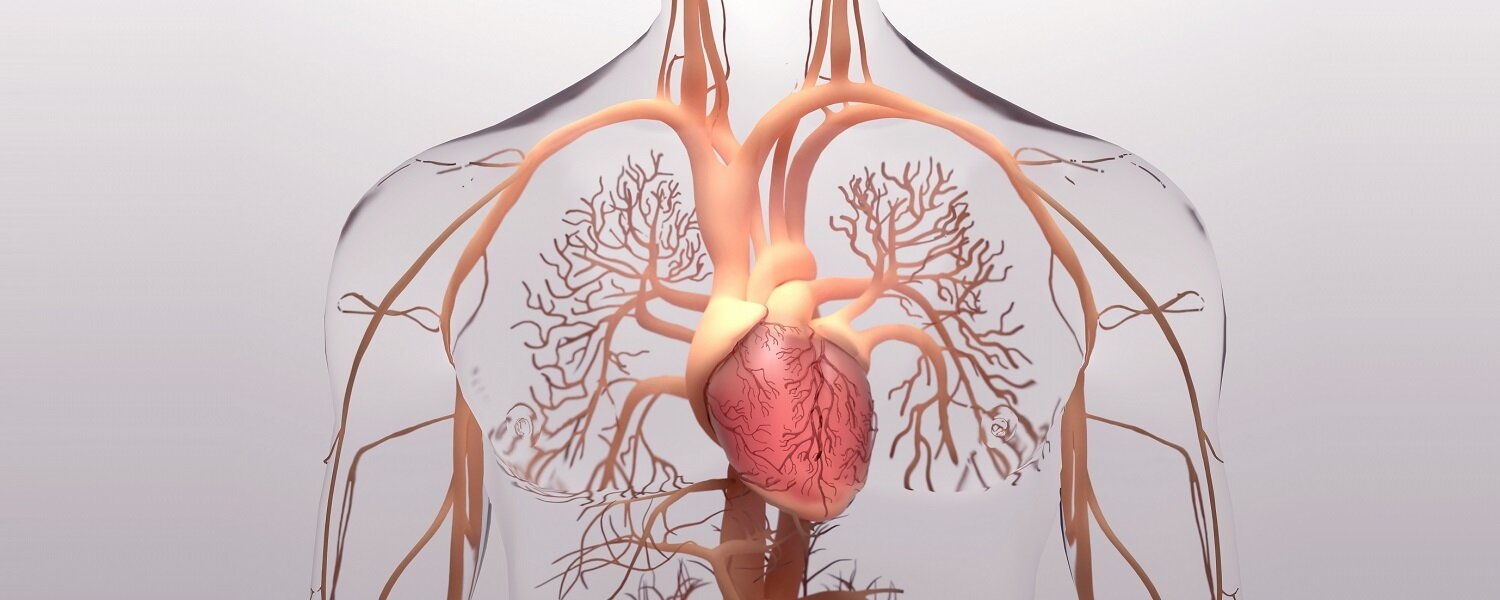
Cardiovascular disease (CVD) is one of the leading causes of mortality and morbidity worldwide, with an estimated 17.9 million people dying from CVD in 2019, representing 32% of all global deaths (1).
Various risk factors are known to contribute CVD, including physical inactivity, type 2 diabetes mellitus, age, gender, genetics, tobacco, and alcohol abuse and a Western-style diet. The impact of animal source foods (ASF), including unprocessed red meat, processed meat, fish, poultry and eggs, on CVD has been widely studied. Epidemiological evidence suggests that high intake of processed and unprocessed red meat is associated with CVD, while poultry and fish intake are not (2,3,4).
Several ingredients and mechanisms have been proposed to explain the potentially harmful effects of red meat intake on CVD. These include contents of saturated fat, cholesterol, haem iron in red meats, sodium, nitrites, and high-temperature cooking of processed meats (5,6,7). However, the mechanisms underlying the potential effects of animal proteins remain unclear.
Emerging evidence suggests the gut microbiota may be a key factor linking red meat consumption and other modifiable risk factors (e.g. diet, obesity, inactivity and stress) to CVD (8,9,10). Gut microbiota-generated metabolites such as trimethylamine-N-oxide (TMAO) potentially participate in these linkages (11,12). TMAO is generated by microbial metabolism of dietary L-carnitine (abundant almost exclusively in red meat) (13) and choline (present in various ASF) (14). Specific gut microbial enzymes primarily metabolise these dietary precursors to produce high levels of trimethylamine (TMA). TMA is further absorbed into the bloodstream and oxidised in the liver by flavin monooxygenases (FMOs, mainly FMO3) to generate TMAO (12). In addition, two intermediates are also produced by gut microbial metabolism of L-carnitine, and these can be further converted to TMAO (15).
Large-scale clinical cohort studies have demonstrated the association of circulating TMAO with death from cardiometabolic diseases, including diabetes (16), chronic kidney disease (17,18,19), and CVD (20,21,22), and all-cause mortality (23). However, whether TMAO and other metabolites derived from L-carnitine may help explain the effect of red meat intake on cardiovascular risk and to what extent they are involved in the cardiovascular risk of high meat consumption is still unknown.
A recent prospective cohort study of 3,931 adults (>65 years) in the United States investigated ASF intake and TMAO-related metabolites over a median of 12.5 years (15).
After adjusting for sociodemographic factors, lifestyle, dietary factors, and antibiotics use, total meat intake was associated with 22% higher incidence of CVD for every 1.1 serving per day. Nearly eight per cent of this elevated risk was mediated by the levels of the three-gut microbiota-generated metabolites of dietary L-carnitine (TMAO, γ-butyrobetaine, and crotonobetaine).
Higher intake of unprocessed red meat and total ASF were associated with 15% and 18% higher incidence of CVD, respectively. TMAO metabolites significantly mediated these risks by 10.6% and 9.2%, respectively.
Processed red meat intake was associated with a nonsignificant trend toward higher CVD risk. There were no associations between CVD risk and fish, poultry, and egg consumption.
After evaluating traditional CVD risk factors as mediators, neither blood cholesterol nor blood pressure levels mediated the relationship between CVD risk and total meat consumption. However, factors that significantly mediated the total meat-CVD association included blood glucose (26.1%), insulin (11.8%), and C-reactive protein (6.6%).
In vitro and animal studies demonstrate that TMAO has several mechanisms that may contribute to CVD:
- Promotes cholesterol accumulation in macrophages by upregulating cell surface expression of proatherogenic scavenger receptors (24,25).
- Inhibits reverse cholesterol transport and alters sterol metabolism (13).
- Induces platelet hyper-reactivity, enhancing thrombotic potential via amplified intracellular Ca2+ release (26).
- Impairs endothelial function by increasing super-oxide-associated oxidative stress and reducing endothelial nitric oxide synthase activity (27).
- Enhances vascular inflammation through activation of mitogen-activated protein kinase and nuclear factor-κB signalling (28) and inflammasome activation (29).
- Inhibits bile acid synthesis, which can trigger an inflammatory response linked to hypercholesterolemia, insulin resistance, atherosclerosis, and heart failure (30,31,32).
Conclusions
The study was observational, and therefore could not control for all risk factors for CVD and may not prove cause and effect between meat consumption and CVD or its mediation by gut microbe-generated chemicals. However, the findings add to the growing evidence linking gut microbiota and CVD and other chronic diseases.
Furthermore, the study indicates that the higher risk of atherosclerotic CVD associated with red meat intake was also partially mediated by glucose-insulin homeostasis and systematic inflammation. Therefore, dietary changes towards a more plant-based or Mediterranean diet (33,34,35,36,37) and interventions targeting the gut microbiota, such as prebiotics and probiotics (38,39), may be important for modulating TMAO and reducing CVD risk. Future studies are required to test the mechanistic relevance of TMAO in CVD and clarify potential diet and microbiome-targeted therapeutics.